Overview of Update Claims - Rebilling
A provider performs a procedure and bills the patient's insurance carrier for the
cost of the procedure. If the patient cancels or deletes the insurance coverage before you
create a claim, the ![]() icon appears on the Patient Overview
window. Depending on the billing order assigned to the procedure, the
icon appears on the Patient Overview
window. Depending on the billing order assigned to the procedure, the ![]() icon appears
next to the following links:
icon appears
next to the following links:
- The primary insurance link if you cancel or delete the primary insurance coverage.
- The secondary insurance link if you cancel or delete the secondary insurance coverage.
- Both primary and secondary insurance links if you cancel or delete both the coverages.
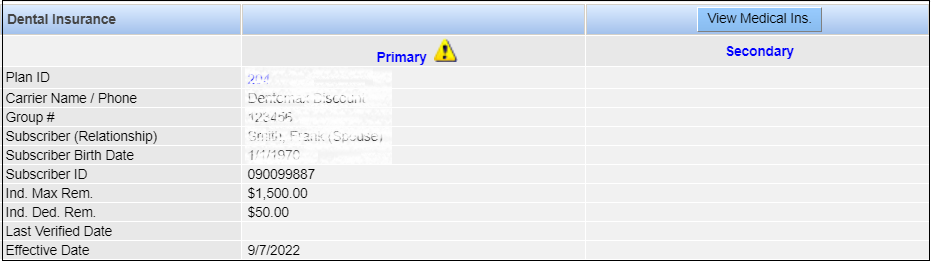
In the following example, the patient has a primary insurance plan.
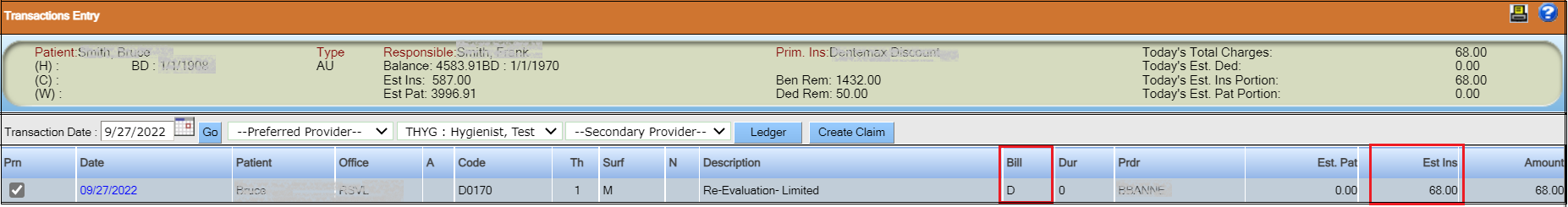
On the Transaction Entry window, the procedure shows "D" in the Bill column indicating that the entire cost of the procedure is billed to the primary insurance carrier.
Now, if we learn the patient was not covered by this insurance for this service date, the
![]() icon
appears next to the primary insurance plan in the Dental
Insurance section.
icon
appears next to the primary insurance plan in the Dental
Insurance section.
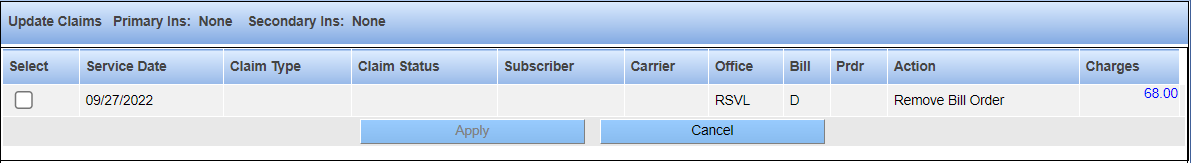
Clicking the ![]() icon opens the Update Claims window.
This window displays the charges you must remove from the primary insurance carrier and
bill to the patient.
icon opens the Update Claims window.
This window displays the charges you must remove from the primary insurance carrier and
bill to the patient.
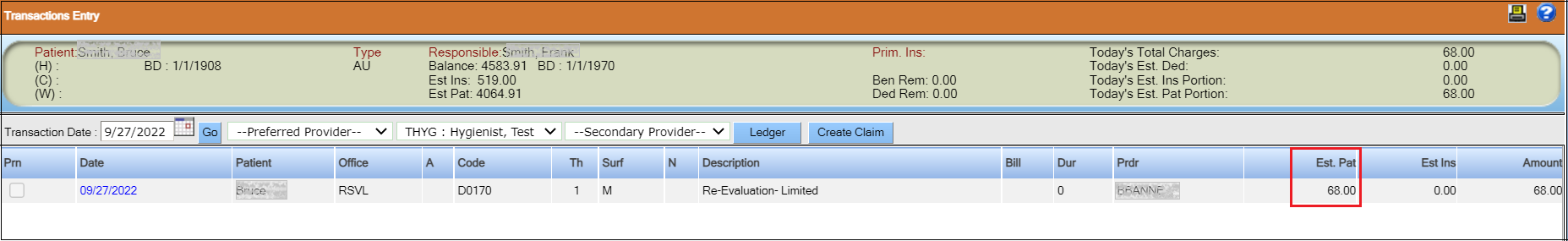
After you perform the remove the bill order action, the entire cost of the procedure is now billed to the patient instead of the insurance carrier.