As claims are paid using the Batch Insurance Payment module, they are tracked at the bottom of the window in the Paid Claims section.
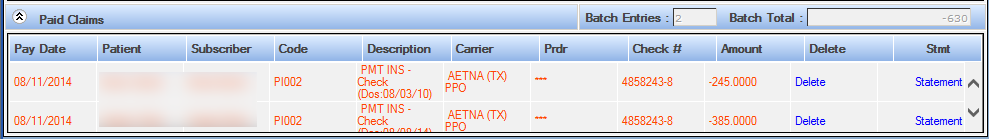
Pay Date: The pay date that was entered in the Patient Insurance Payment section.
Patient: Name of the patient associated with the claim.
Subscriber: The name of the insurance subscriber. This is not necessarily the name of the patient.
Code: The ADA service or Practice Code for the treatment
Description: The description associated with the service code.
Carrier: The name of the insurance plan carrier from whom payment is expected.
Provider: The provider that is associated with the claim. The Provider ID is established in the Provider Setup tool. If more than one provider is represented, *** will appear.
Check #: The check number entered in the Batch Insurance Check Detail section.
Amount: The total amount applied to the claim, calculated as the total paid for the treatments and displayed in the Patient Insurance Payment section.
Delete: Click the delete link to remove the allocation to the specific claim. A confirmation window will appear before the deletion is performed.
Statement: Send a specific individual statement to this patient by printing and processing it locally.