The specifics of the treatments associated with the selected claim.
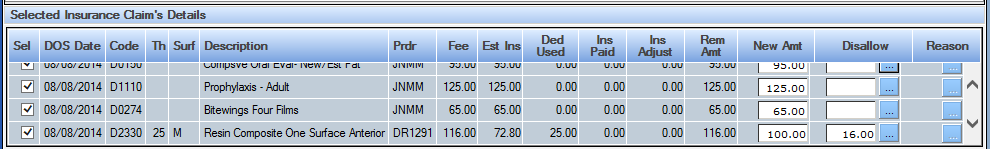
Sel (Select): Click this box to select the specific treatment for payment. The fee is automatically inserted as the amount paid when selected.
DOS Date: Date the treatment was performed
Code: The ADA service or Practice Code for the treatment
Th (Tooth): The tooth associated with the treatment if applicable.
Surf (Surface): The surface associated with the treatment if applicable.
Description: The description associated with the service code.
Provider: The provider that performed the treatment. The Provider ID is established in the Provider Setup tool.
Fee: Fee charged for the service
Est Ins (Estimated Insurance): The estimated portion of the treatment to be paid by the insurance carrier.
Ded Used (Deductible Used): The amount charged toward the patient’s deductible
Ins Paid (Insurance Paid): The amount paid by the insurance to date for the treatment.
Ins. Adj (Insurance Adjustments) The amount of adjustments made to the treatment.
Rem Amt (Remaining Amount): The amount remaining to be paid for the treatment.
New Amt (New Amount): The amount paid by the insurance carrier.
Disallow: The amount being disallowed by the carrier for the specific treatment. An adjustment can be applied for the single treatment as opposed to the full claim level (in the top section.)
Reason: Log the reason codes that indicate why a treatment was disallowed. It doesn’t appear directly in the ledger, but is captured for analysis via the QSIDental Web nightly download.
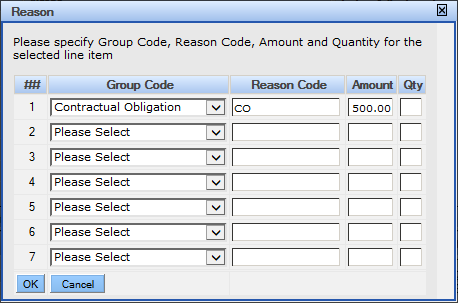
Note: The quantity field is part of the standard 835 communication and would be one in nearly all dental remittances.