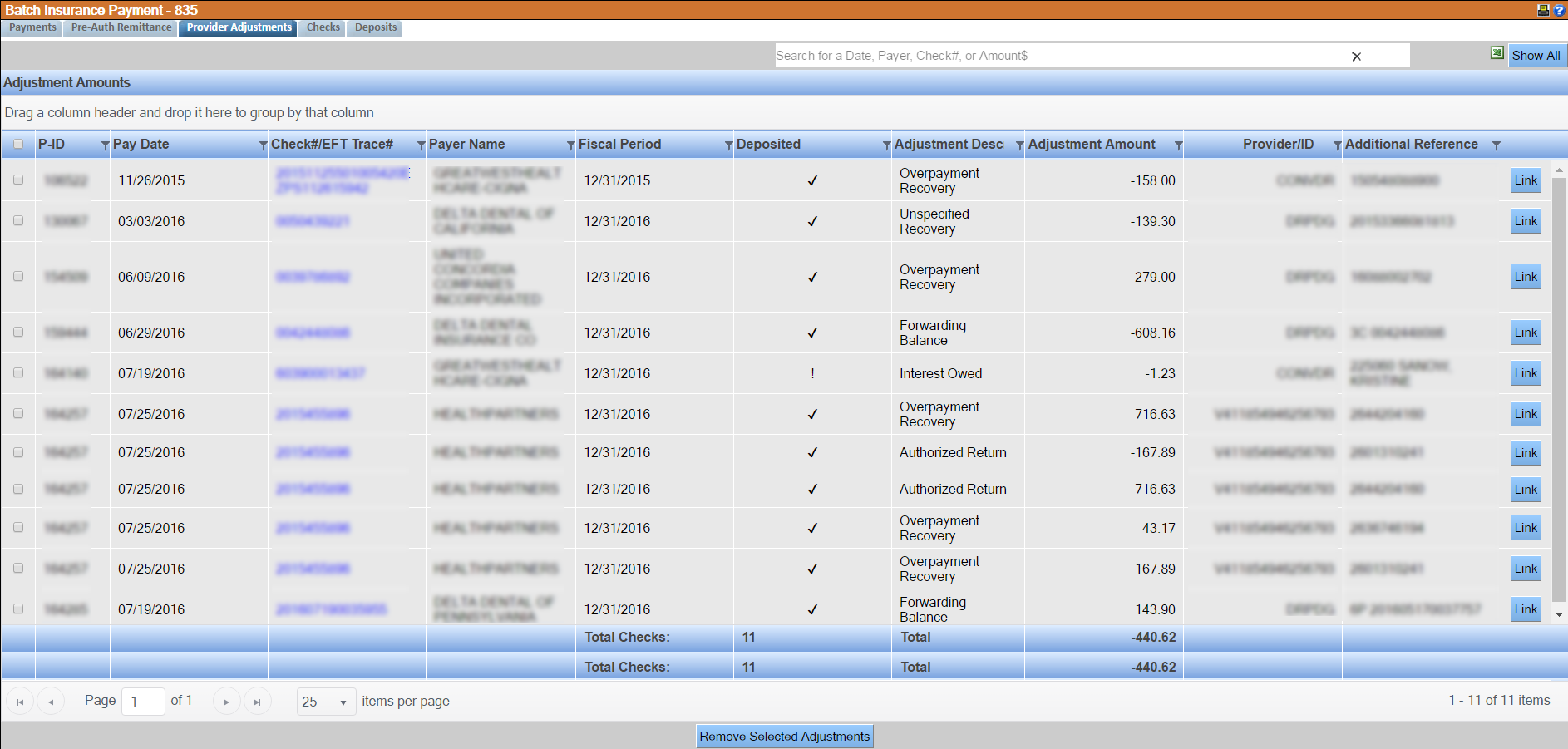
Provider Adjustments Tab
Payments may include some specialized adjustments which are made at the provider level and are independent of specific treatments or claims. These adjustments may increase or decrease the amount paid on a check. While the adjustment is not always associated with a specific claim in the 835, they are used to balance the transactions. Possible provider adjustments include:
- Increased payment for a provider incentive plan
- Increased payment from interest from a late payment
- Increased payment for a loan repayment
- Reduced payment because of a prior overpayment
The Provider Adjustments tab displays all of the checks that contain a provider adjustment and the details of each adjustment. While the payments will still be posted for the corresponding claim and will not be held back, corresponding adjustments can be made.
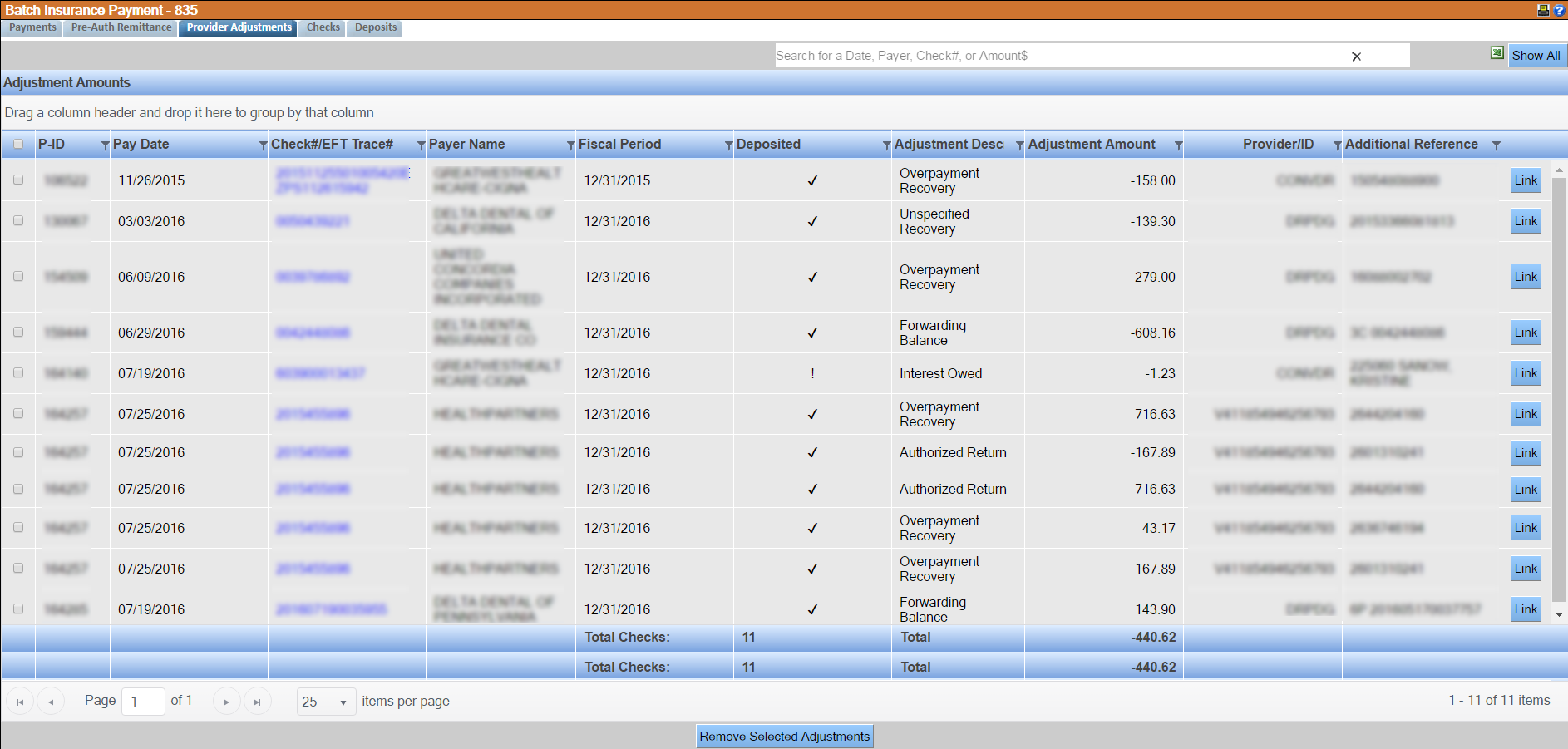
The Provider Adjustments tab displays some details for the check, its associated payment, and the provider adjustment itself depending on the radio button selected to filter the list. The details include:
- P-ID: The Claim Header Identifier for the check.
- Pay Date: The date of the payment.
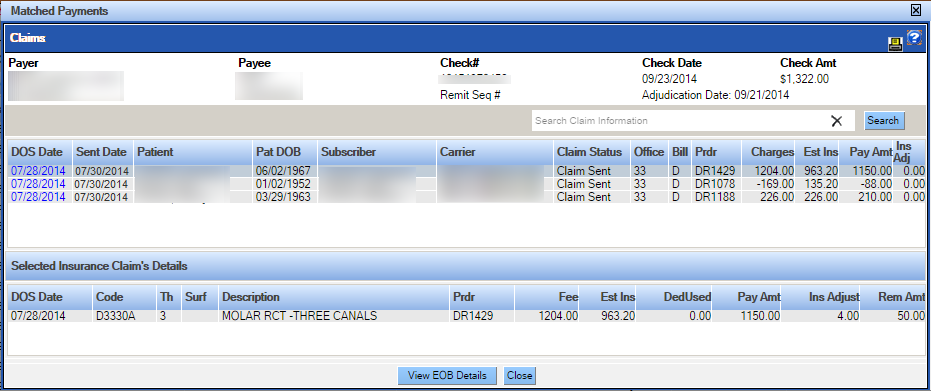
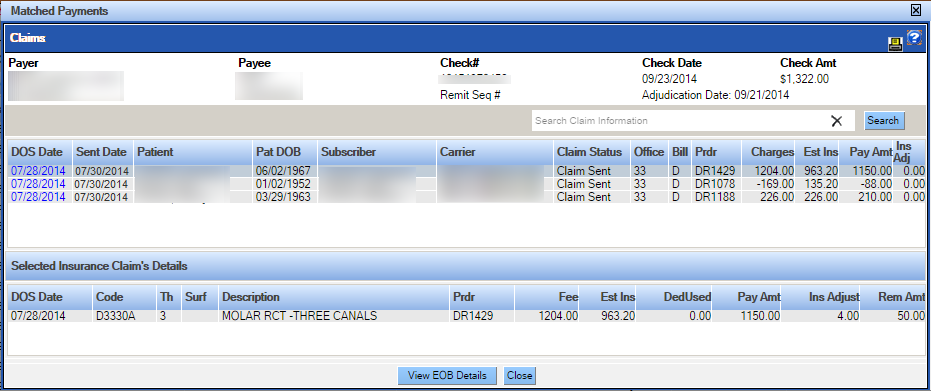
- Check#/EFT Trace #: If the adjustment payment was delivered as a check, the check number will display; if payment was made using an electronic funds transfer (EFT), the EFT number will display. This identifier number is setup as a hyperlink and when clicked, will open a window identifying all claims and line items associated with the payment. It can be used to identify and evaluate allocations made.
- Payer Name: Carrier that issued the adjustment.
- Fiscal Period: The date which ends the provider’s fiscal period, according to the 835 file.
- Deposited: Indicates whether a check/EFT payment was received. Displays as a checkmark or exclamation point to match the detail of the check from the imported deposit file.
- Adjustment Description: A short summary of the reason for the adjustment.
- Adjustment Amount: The amount of the adjustment for the identified issue
- Provider/ID: The provider associated with the adjustment. If the provider can be mapped to a provider in QSIDental Web, that provider number will display, if not, the provider number will display as indicated in the file.
- Additional Reference ID: On occasion, the adjustment will be associated with a previously paid claim. In these cases, if the reference number provided can be tied to an existing claim within QSIDental Web, the patient number and name associated with that claim will display, if not, the reference number will display as indicated in the file.
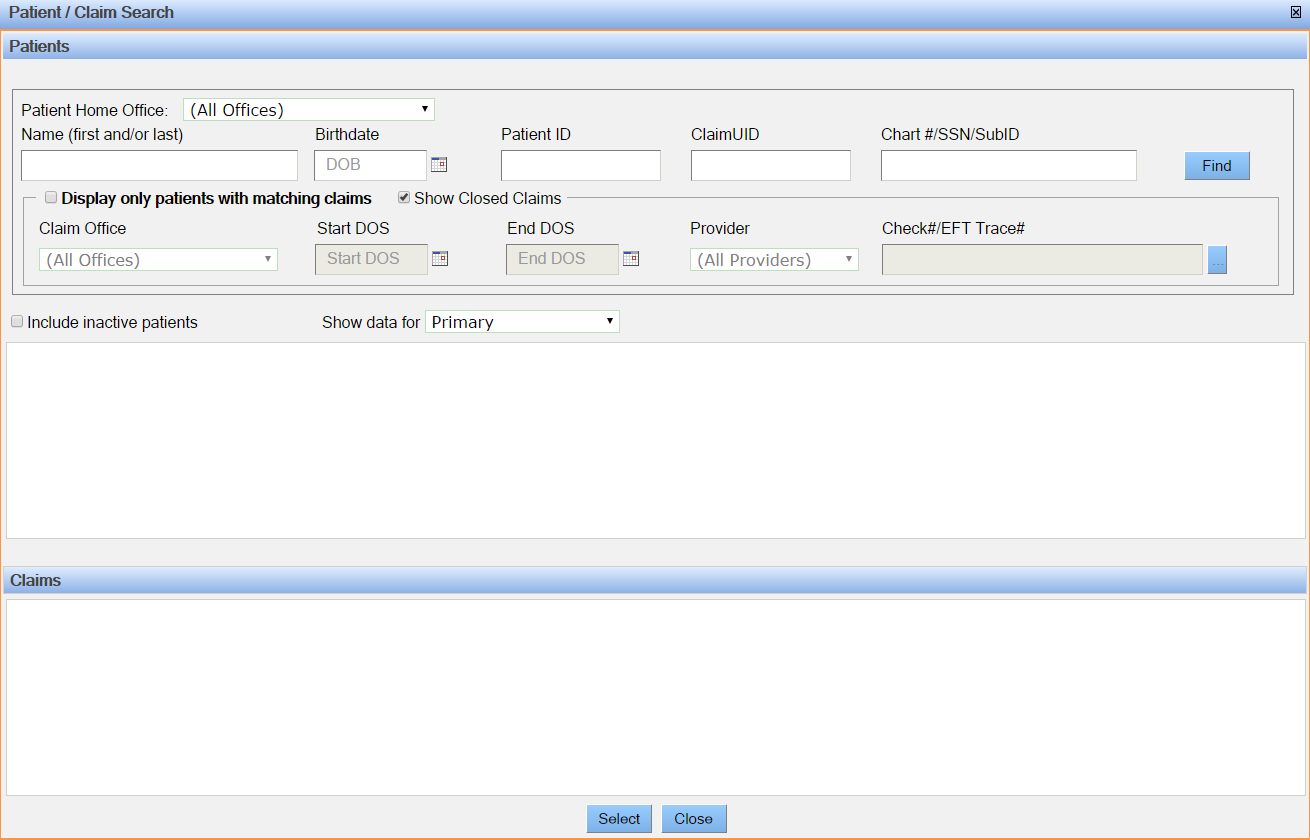
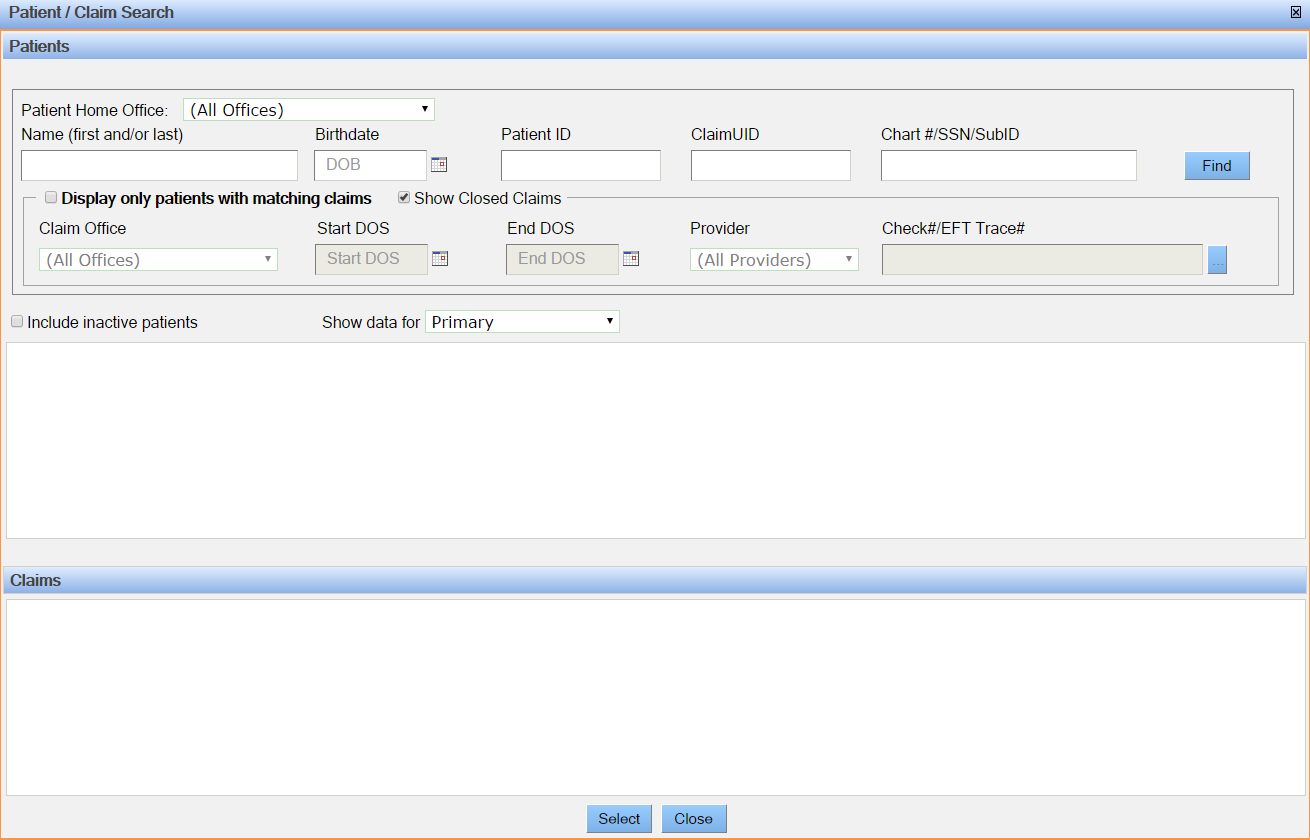
- Link button: Opens the Patient claim search window. From here select one or more provider adjustments that are linked to a claim.
- Remove Selected Adjustment button: Clicking this button removes the selected adjustments from the window. Once the adjustment is removed it cannot be linked to a claim.
The items on this window appear for information only. Increases or decreases must be manually applied in accordance with practice policies. When posting these adjustments, please note that:
- Positive adjustment amounts decrease the total check amount.
- Negative adjustment amounts increase the total check amount.