Overview of Service Restrictions
About Service Restrictions
Many insurance carriers have limitations and restrictions on the procedures that will be covered for a given patient. For example, one carrier might cover only two cleanings a year, while another might cover three. Knowing whether or not a procedure will be covered helps both provider and patient make informed decisions.
QSIDental offers an optional Service Restrictions function for QSIDental Web to determine if a procedure will be covered given a specific carrier’s rules and the patient’s circumstances.
Rule Types
There are six rule types that are prevalent among carriers. These rules are preloaded to the Service Restrictions function, though the individual restrictions need to be added by a QSIDental Web Administrator. For each rule, a carrier will determine the parameters that either restrict or allow coverage for a given procedure. The following chart explains the six key rules and their associated parameters and provides an example for each.
|
Rule |
Parameter |
Example |
|
Not Allowed (age-based) |
Procedures are restricted to or for a specific age or range. |
Sealant will only be covered for patients under 18. |
|
Consent Form |
Consent-based requirement for a procedure. |
Patient informed consent required prior to initiating treatment. |
|
Frequency |
Procedures may only be performed on a limited basis within a plan year. |
Periodic Oral Evaluations will be covered once every six months. |
|
Pre-authorization |
Require the carrier to authorize the procedure in advance. |
Implants will only be covered with prior authorization. |
|
Teeth Based |
Limit a procedure to a specific tooth or teeth. |
Sealants will be covered for Tooth #2, #3, #14, #15, #18, #19, #30 and #31 only. |
|
Time Interval |
Limit to the number of times per period a procedure can be covered. |
Cleanings will only be covered two times per year. |
Service Restriction Alerts
Once service restrictions are set up by an administrator, QSIDental Web will warn users if a planned or completed procedure is within the service restrictions and guidelines. Additionally, users can check specific procedures directly from the chart and also from a treatment plan to see if any service restrictions apply. Either way, QSIDental Web will display an alert detailing the restrictions or indicating that the services are allowed.
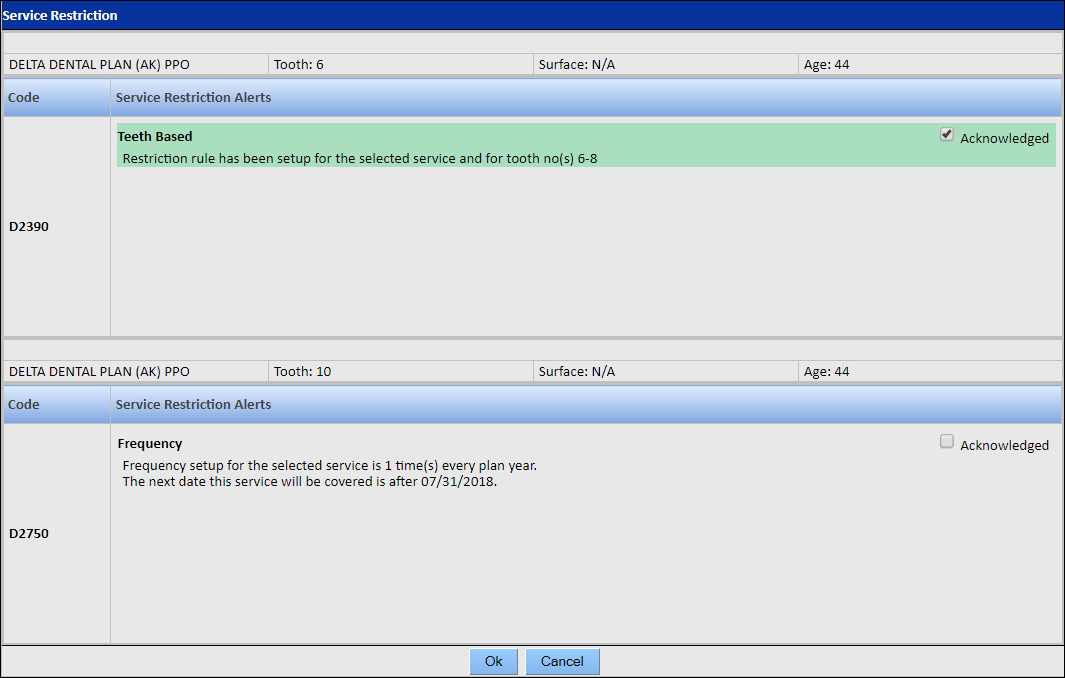
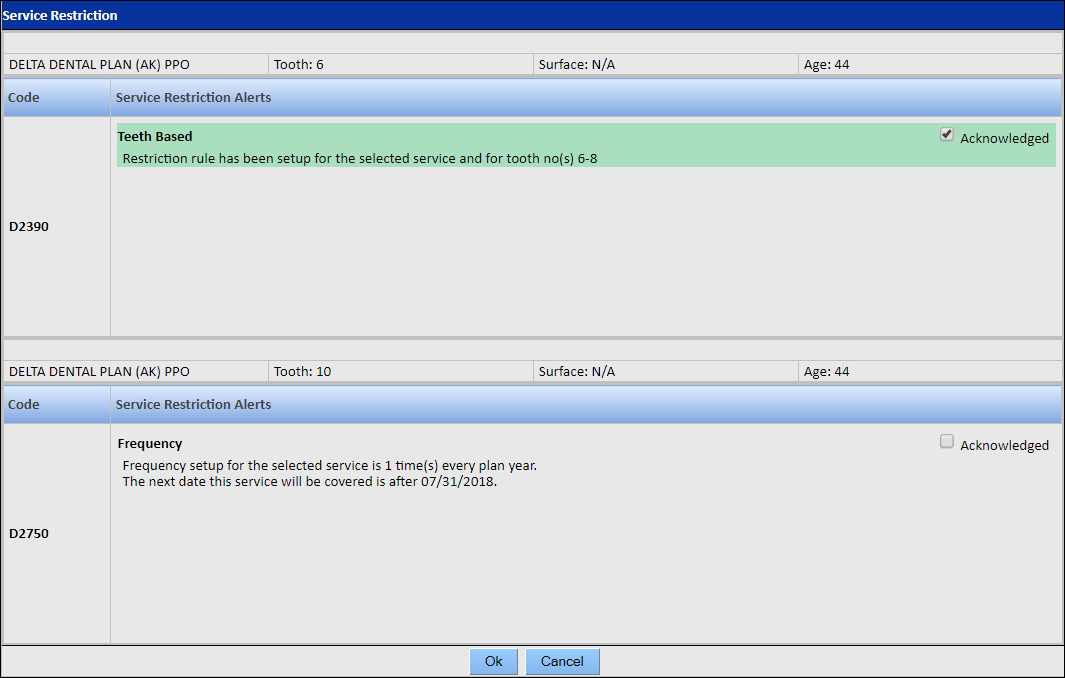
Each alert will provide details regarding the restriction. For example, alerts based on frequency or time-interval restrictions will list the date on which the service will next be eligible for coverage based on information present in the chart history, and tooth-based alerts will state the teeth on which the service may be performed.
Acknowledge a Service Restriction
To acknowledge a service restriction:
-
Select the Acknowledged check box in the service-restriction
alert when it displays.
Note: The alert is shaded green to indicate it has been acknowledged. For example, in the following screen shot, the restriction on procedure D2390 has been acknowledged, while the restriction on D2750 has not. If there are multiple restrictions listed for a single service code, an Acknowledged All check box appears, allowing you to acknowledge all of the service restrictions at once.
-
Click OK.
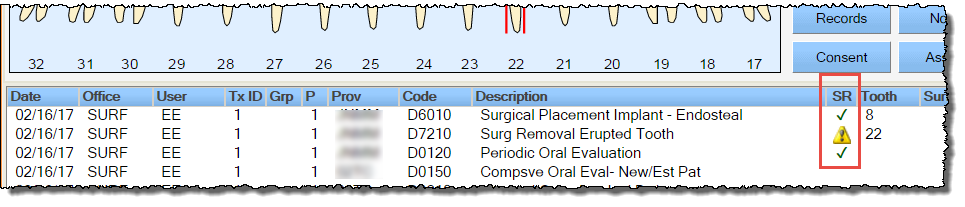
Now that the service restriction is acknowledged, a check mark appears for that service in the SR column of the Chart Details section of the Tooth Chart and also in the patient's treatment plan. An alert icon appears for service restrictions that have not been acknowledged. For example, in the following screen shot, service codes D6010 and D0120 have service restrictions that have been acknowledged, while service code D7210 has a service restriction that has not been acknowledged.
 Note: If a procedure has unacknowledged service-restriction alerts, it can still be planned and completed; however, the procedure may not be covered by the carrier.
Note: If a procedure has unacknowledged service-restriction alerts, it can still be planned and completed; however, the procedure may not be covered by the carrier.
