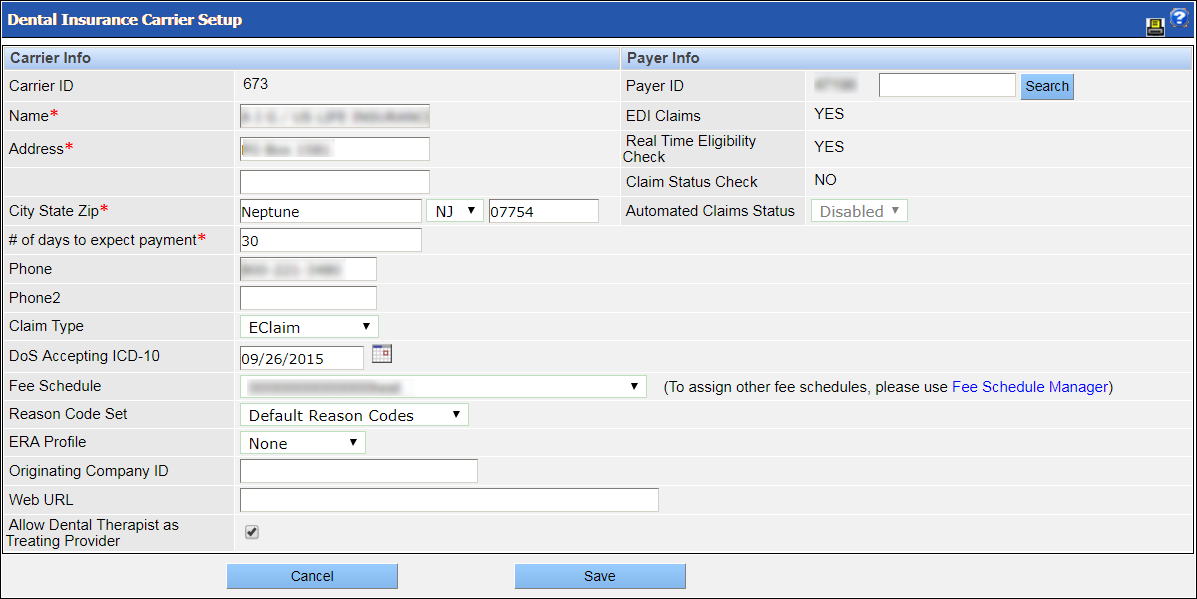
Insurance: Dental Carriers
The Dental Insurance Carrier Setup screen allows a practice to set up and manage a database of dental carriers. These carriers will appear in the dropdown list of carriers when a user is creating an insurance plan.
Following are descriptions of the fields you see on the Dental Insurance Carrier Setup screen when you are adding or editing a carrier:
Carrier Info
- Carrier contact information: The carrier's name, address and phone numbers.
- # of days to expect payment: The number of days within which you should expect payment to be made by the carrier. This value is used in automatic claim status checks. If automated claims status check is enabled for the payer, the system will send an automated claim status request if payment has not been received by the specified number of days. This value is also used to compute the follow-up date for the Claim Worklist feature.
- Claim Type: The type of claim submitted to the carrier, such as e-claim or paper claim.
- DoS Accepting ICD-10: The date the carrier began accepting ICD-10 diagnosis codes.
- Fee Schedule: The fee schedule used by the carrier as defined on the Fee Schedule Setup screen.
- Reason Code Set: The reason code set used by the carrier as defined on the Reason Code Setup screen.
- ERA Profile: The ERA profile of the carrier as defined on the ERA Profile screen.
- Originating Company ID: The ID of the carrier's originating company.
- Web URL: The URL of the carrier's website.
- Allow Dental Therapist as Treating Provider: Allows procedures that are completed by a dental therapist or advanced dental therapist to be submitted in claims or preauthorizations.
Payer Info
- Payer ID: The carrier's payer ID. This field is critical, especially when electronically filing claims. To populate this field, you must search for a payer by entering all or part of the payer ID or the payer name and then clicking Search. To help with your search, you can look up a payer ID in the Carrier Payer ID list, which you can access from the Help menu.
- EDI Claims: Indicates whether or not the payer accepts EDI claims. This value is taken from NextGen EDI and is not editable.
- Real Time Eligibility Check: Indicates whether or not the payer provides real-time eligibility check. This value is obtained from NextGen EDI and is not editable.
- Claim Status Check: Indicates whether or not the payer provides claim-status check. This value is taken from NextGen EDI and is not editable.
- Automated Claims Status: Indicates whether or not the payer provides automated claim-status checks. If the value of the Claim Status Check field is Yes, the Automated Claims Status field will be available for editing. If you select Enabled, the system will automatically send a request for claim status after the number of days entered in the # of days to expect payment field.