Practices that subscribe to NextGen Healthcare's Electronic Data Interchange® (EDI) service can check eligibility electronically on an as-needed basis. An insurance eligibility report details the response from the carrier.
Note: Insurance last verified dates displaying in red indicate it has been more than 30 days since an eligibility verification was performed.
The Patient Eligibility window displays.
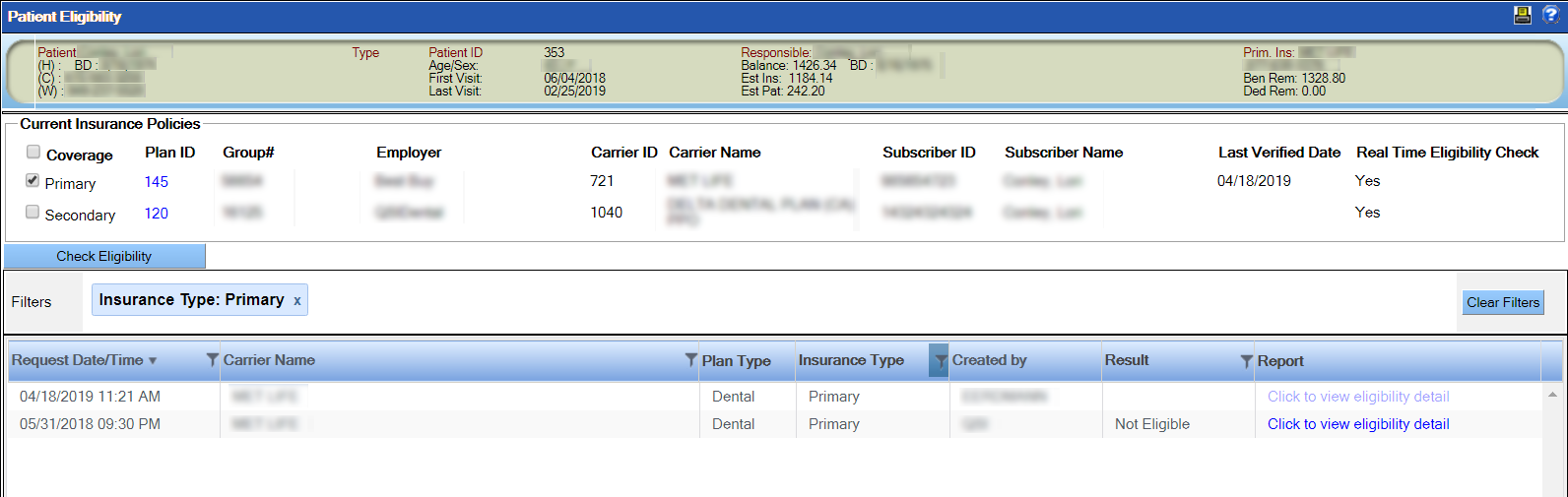
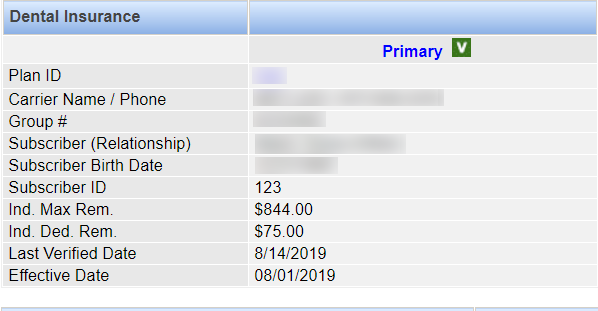
Note: To view details about a patient's primary or secondary insurance plan, click the plan ID.
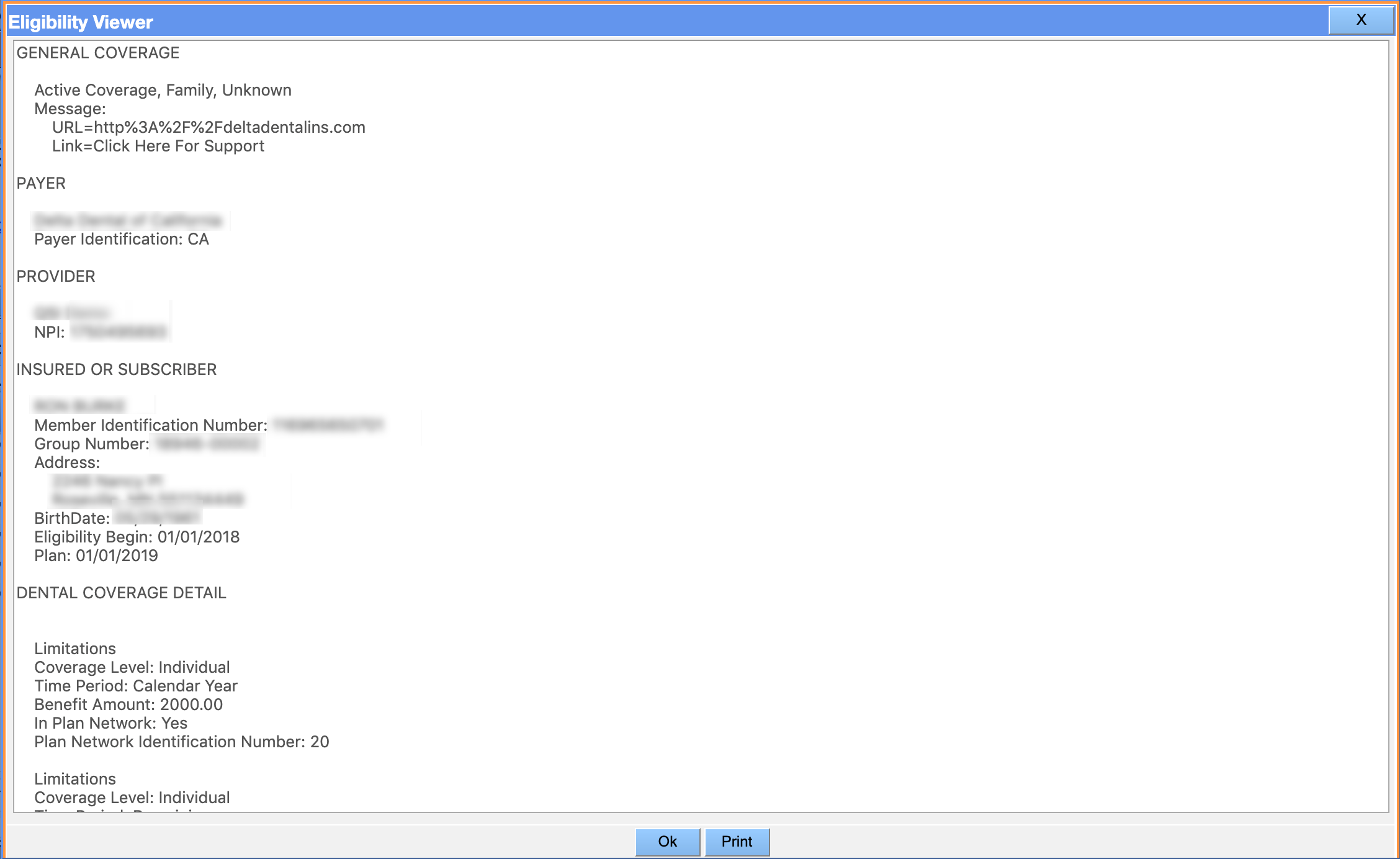
The system submits a request for an eligibility check and logs the request in the history in the lower half of the window. When a response is received from EDI, the result will appear in the history, and you will be able to view and print the eligibility report by clicking the link in the Report column. If applicable, the patient's status will also change to verified.